Notes from the field: Pain sensitivity before, during, and after migraine

Uglem M, Omland PM, Nilsen KB, Tronvik E, Stovner LJ, Hagen K, et al. Does pain sensitivity change by migraine phase? A blinded longitudinal study. Cephalalgia (2017); 37:1337–49.

Background: Setting the scene
Altered pain perception has been implicated in migraine pathophysiology.1 It has been shown that experimental pain thresholds decrease with a subsequent increase in pain scores for people living with migraine even in the interictal phase, compared to healthy controls.1 Furthermore, studies have shown an increased response to pain during the ictal phase compared with the interictal phase.2 This study aimed to investigate whether pain thresholds decrease and pain scores increase on the day before, during, and the day after an ictal phase, compared with an interictal phase. Specifically, the investigation focused on whether suballodynia (a pain threshold decrease within the normal range) and/or hyperalgesia (increased sensitivity to pain) precedes and outlasts headache during a migraine attack, and if people living with migraine had increased suprathreshold pain scores compared with headache-free controls during the interictal phase.

Study summary
STUDY DESIGN HIGHLIGHTS
The study included 50 people living with episodic migraine and 31 headache-free controls who were primarily women (84%) across both groups, with a mean age of 38 and 40 years, respectively. This was a longitudinal blinded study where investigators were unaware of participants’ migraine diagnoses a well as their respective migraine phases during their study visits.
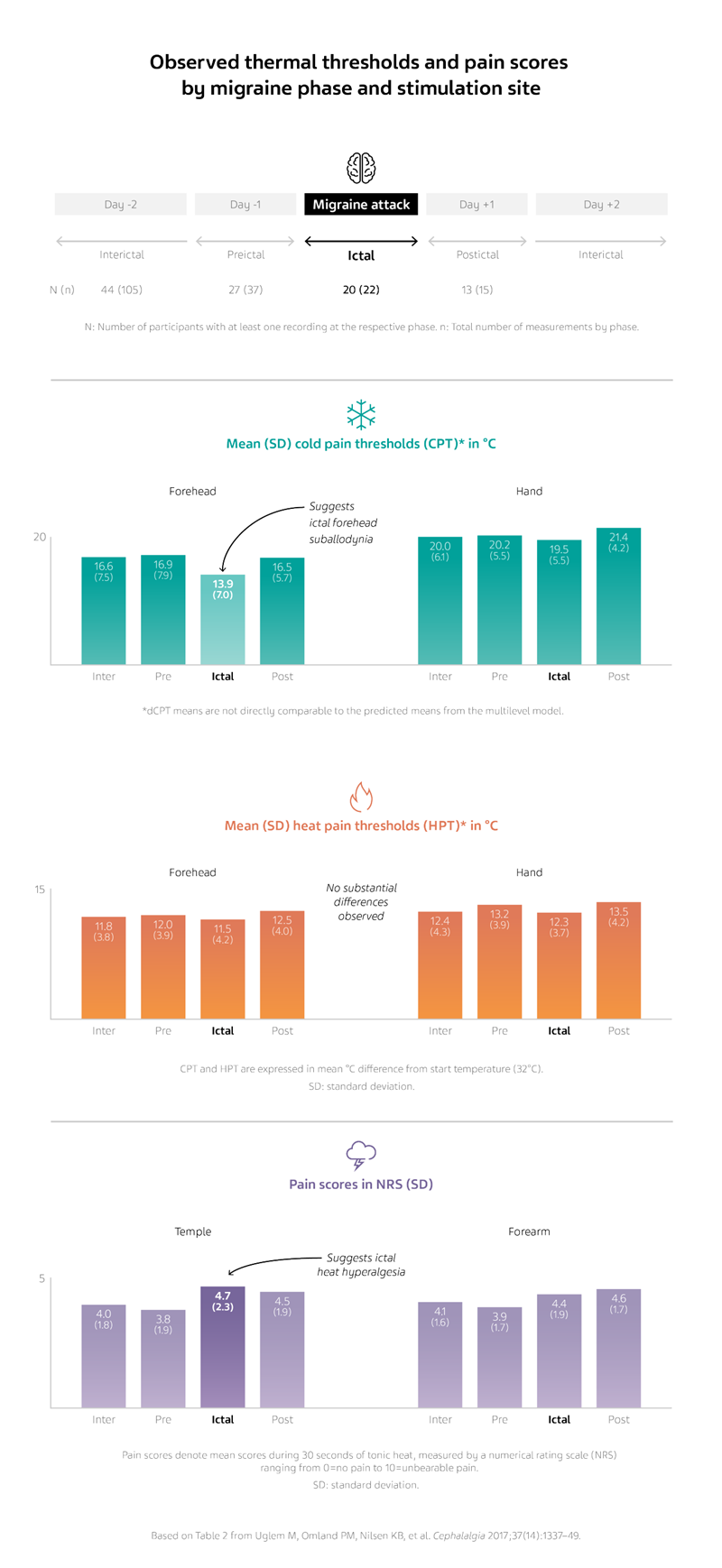
Thermal pain thresholds to cold and heat, and pain scores during 30 seconds of suprathreshold heat, were measured four times in those with migraine, and once in headache-free controls. Participants with migraine also completed a headache diary for 4 weeks before, during, and 4 weeks after the study visits to determine the relation of symptoms with different phases of a migraine attack. For participants with migraine, study visits were categorized in their migraine diaries as interictal, preictal (≤1 day before an attack), ictal, or postictal (≤1 day after an attack).
Thermal pain threshold recordings were performed on the right hand and right side of the forehead using a handheld thermode, and participants were instructed to press a button when the stimulus was perceived as painful. Temporal profiles of suprathreshold heat pain scores were obtained through a continuous suprathreshold heat pain stimulation on the right forearm and temple for 30 seconds. Pain scores were verbally reported by participants using a numerical rating scale (NRS), continuously throughout stimulation.
RESULTS HIGHLIGHTS
Forehead cold pain thresholds were significantly decreased in the ictal phase compared with the interictal phase. The decrease was within the normal range, and thus interpreted as trigeminal suballodynia in the ictal phase. On the other hand, no significant differences were established between heat pain thresholds regardless of migraine phase or stimulation site.
Overall pain scores from stimulation at the temple during continuous suprathreshold heat pain stimulation increased in the ictal phase compared with the interictal phase, and was interpreted as trigeminal hyperalgesia in the ictal phase.
When pain scores were further analyzed throughout the 30 seconds of stimulation, preictal pain scores decreased compared with interictal pain scores at both the temple and forearm at the initiation (time point 0 seconds) of suprathreshold heat pain stimulation, which was interpreted as initial preictal hypoalgesia. At both stimulation sites, there were interictal decreases in pain scores from 0 seconds to 20 seconds and 0 seconds to 30 seconds, which was interpreted as interictal adaptation of pain scores. Within those timepoints, preictal pain scores decreased significantly less compared with interictal pain scores, and this was interpreted as preictal lack of adaptation.

Conclusions and future implications
This longitudinal investigation examined experimental pain in patients with migraine during four different phases of headache, and clinically assessed relevant pain-physiology parameters such as allodynia, hyperalgesia, and hypoalgesia. These results, in addition to temporal summation by each migraine phase within a migraine cycle, help to strengthen our understanding of the cyclic alterations of pain perception in patients with migraine. Trigeminal cold suballodynia and heat hyperalgesia were found during the ictal phase of headache, and heat hypoalgesia as well as reduced adaptation to suprathreshold heat pain were identified preictally in both trigeminal and peripheral sites. The study suggests that an interictal-preictal-ictal gradient can exist for both CPT (cold pain threshold) and HPT (heat pain threshold), and that central changes in pain physiology appear to emerge during the preictal phase—this is possibly related to headache-initiating mechanisms.
References
- Schwedt TJ, Krauss MJ, Frey K, Gereau RW. Episodic and chronic migraineurs are hypersensitive to thermal stimuli between migraine attacks. Cephalalgia 2011;31(1):6–12.
- Moulton EA, Becerra L, Maleki N, et al. Painful heat reveals hyperexcitability of the temporal pole in interictal and ictal migraine States. Cereb Cortex 2011;21(2):435–48.
NPS-US-NP-01551









